Insulin, Inflammation & Cortisol: Why Blood Sugar Balance Matters for Your Brain and Body
We often think of insulin resistance as something that only matters if you have diabetes. But here’s the truth: insulin sensitivity is at the center of your energy, mood, sleep, gut health, and even how your brain responds to stress. When insulin gets thrown off, it creates ripple effects that can leave you feeling foggy, anxious, and inflamed.
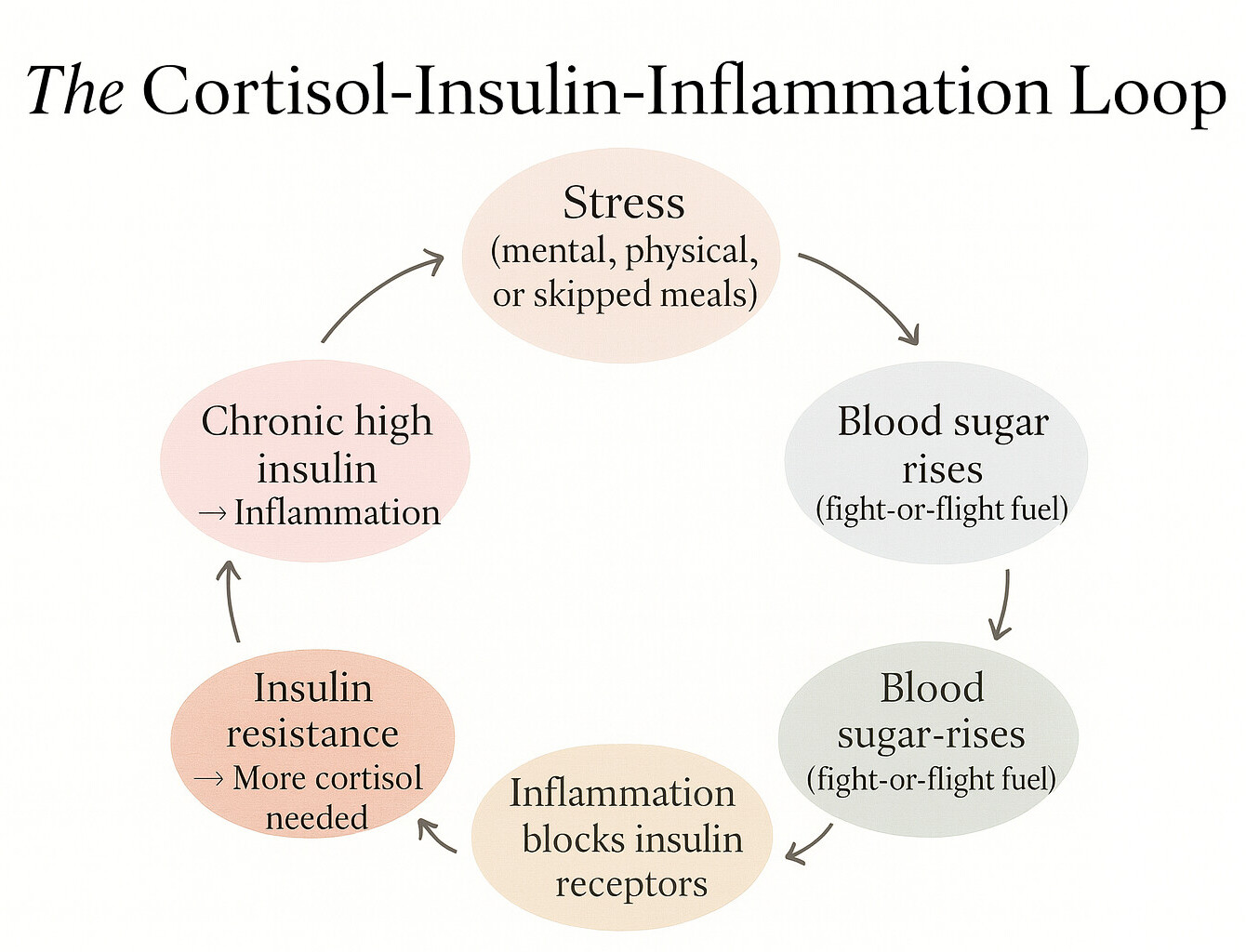
The Blood Sugar–Cortisol Dance
Your body has a backup plan for unstable blood sugar, and it’s called cortisol.
- When blood sugar spikes too high (after a refined carb or sugary meal) or drops too low (from skipping meals or under-eating), cortisol is released to stabilize things.
- This release is part of your fight-or-flight response. The adrenal glands release cortisol to mobilize glucose into the bloodstream so your muscles and brain have immediate energy — even if there’s no “bear” to run from.
- Short-term, that’s lifesaving. But when it happens every day (from chronic stress, irregular eating, or under-fueling) cortisol stays elevated.
Why that matters: Cortisol naturally reduces insulin sensitivity so your body can keep glucose circulating during stress. But if cortisol is high all the time, your cells stop listening to insulin effectively, forcing your pancreas to pump out more of it.
How Inflammation Fits In
- When insulin is chronically elevated, it stimulates your immune system to pump out pro-inflammatory cytokines (inflammatory messengers like IL-6 and TNF-α).
- These cytokines then interfere with insulin receptors, making cells even more resistant.
- That means your body has to secrete more insulin to get the job done — worsening inflammation in the process.
It’s a loop: cortisol raises blood sugar → insulin rises → inflammation increases → inflammation blocks insulin → more cortisol is needed to compensate.
The Trickle-Down Effect
Once this loop spins too long, it doesn’t just show up in lab numbers — it shows up in how you feel:
- Mood & stress response: Elevated cortisol shrinks hippocampal neurons, making memory and emotional regulation harder. This can show up as anxiety, irritability, or low mood.
- Sleep: Cortisol spikes at night prevent melatonin from rising, disrupting both falling and staying asleep.
- Gut function: Cortisol changes blood flow and enzyme output in the digestive tract, while inflammation increases gut permeability (“leaky gut”).
- Cognitive function: Insulin resistance reduces glucose uptake in the brain, leading to brain fog and slower thinking.
- Metabolic flexibility: Your body becomes less able to switch between burning carbs and fats efficiently — which isn’t just about weight, but about consistent energy.
How to Know If You’re Insulin Sensitive
You don’t have to guess. A few ways to check in:
Body signals:
- Post-meal crashes or drowsiness
- Intense sugar cravings
- Feeling shaky, anxious, or “hangry” if you go too long without food
Lab markers:
- Fasting insulin (ideal <5 µIU/mL) — often more sensitive than glucose alone
- Fasting glucose (<90 mg/dL ideal, but context matters)
- HOMA-IR score (calculated from insulin + glucose) — >2.0 suggests resistance
- Hemoglobin A1c (reflects 3-month average, but less sensitive for early changes)
- hs-CRP (marker of inflammation)
At-home tracking:
- Continuous glucose monitors (CGMs) like Levels or Nutrisense show how meals and stress affect you in real time
- Even a finger-stick glucometer can help identify patterns
What Helps Break the Cycle
1. Lifting & movement
- Resistance training boosts the “glucose doors” in your muscle cells — making it easier for sugar to move from your bloodstream into muscle for energy, even with less insulin involved.
- Aerobic exercise improves mitochondrial function, which helps cells use energy more efficiently.
- Even a 10–15 minute walk after meals significantly blunts glucose spikes.
2. Eating rhythm
- Regular meals stabilize cortisol output — irregular eating patterns are perceived as a stressor.
- Prioritize protein and fiber: they slow glucose absorption, reducing spikes and crashes.
- Pair carbs with fat or protein: this lowers glycemic response.
3. Anti-inflammatory nutrients
- Magnesium is required for insulin receptor activation and also calms the nervous system.
- Omega-3s reduce pro-inflammatory cytokines and support neuronal resilience.
- Polyphenols (berries, olive oil, turmeric) act as antioxidants and improve endothelial function.
- Vitamin D modulates both insulin sensitivity and HPA axis regulation.
4. Stress recovery
- Breathwork, meditation, or mindful breaks reduce HPA axis overdrive.
- Circadian rhythm support (morning light, regular sleep schedule) lowers evening cortisol.
- Restorative sleep repairs insulin receptor sensitivity.
My Takeaway
When I started connecting the dots between my energy dips and blood sugar swings, it made sense why stress felt so much harder on certain days. A continuous glucose monitor showed me exactly which meals were keeping my blood sugar steady and which ones left me foggy and wired. Adding strength training, more protein, and magnesium has made a noticeable difference in my clarity and calm.
The beauty is that stabilizing blood sugar isn’t about restriction. It’s about steady fuel, steady hormones, and steady mood.
© 2025 Nassif Psychotherapy Co. All Rights Reserved.